Brilliant Synthesis Technology Results High Quality Vaccine Adjuvants
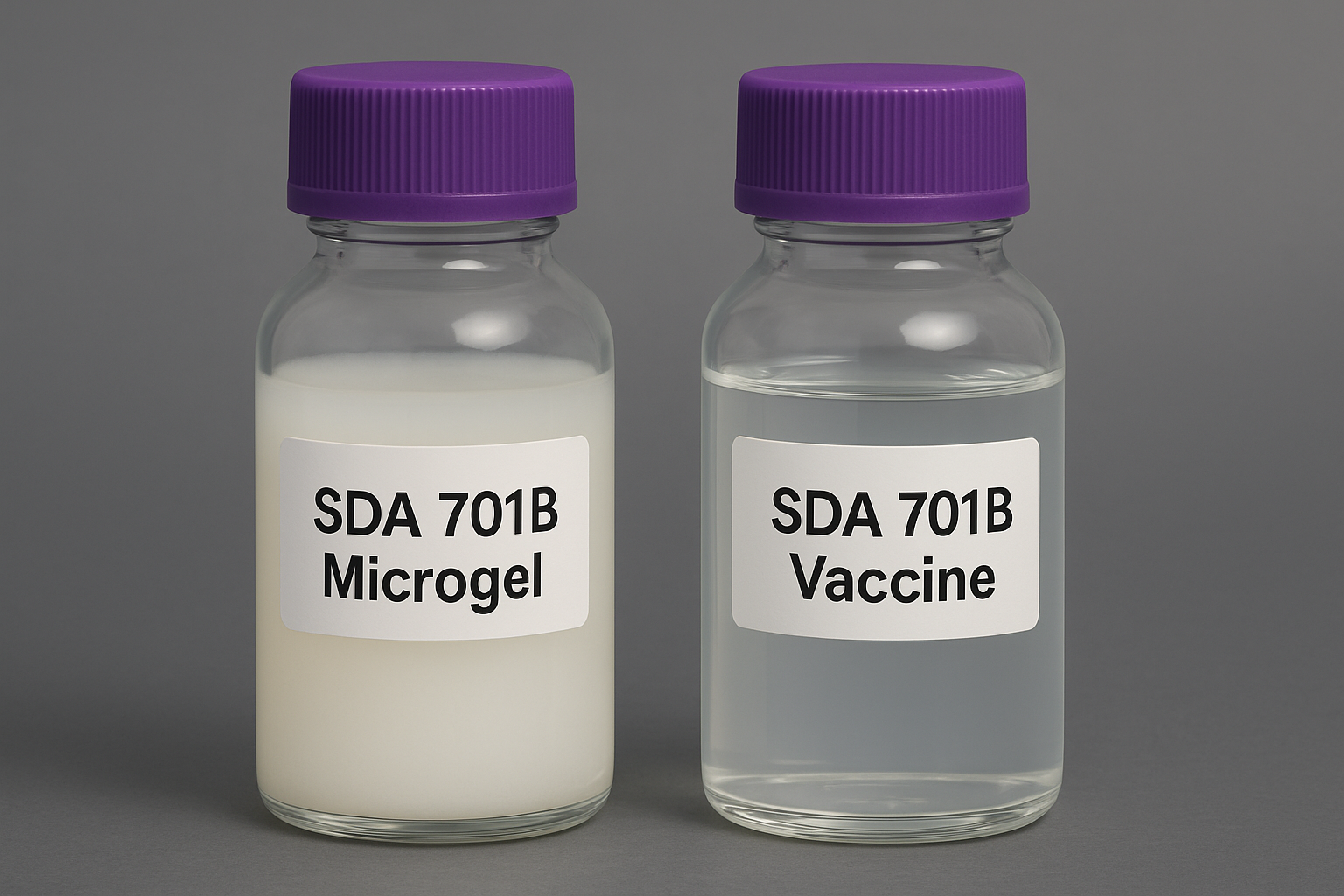
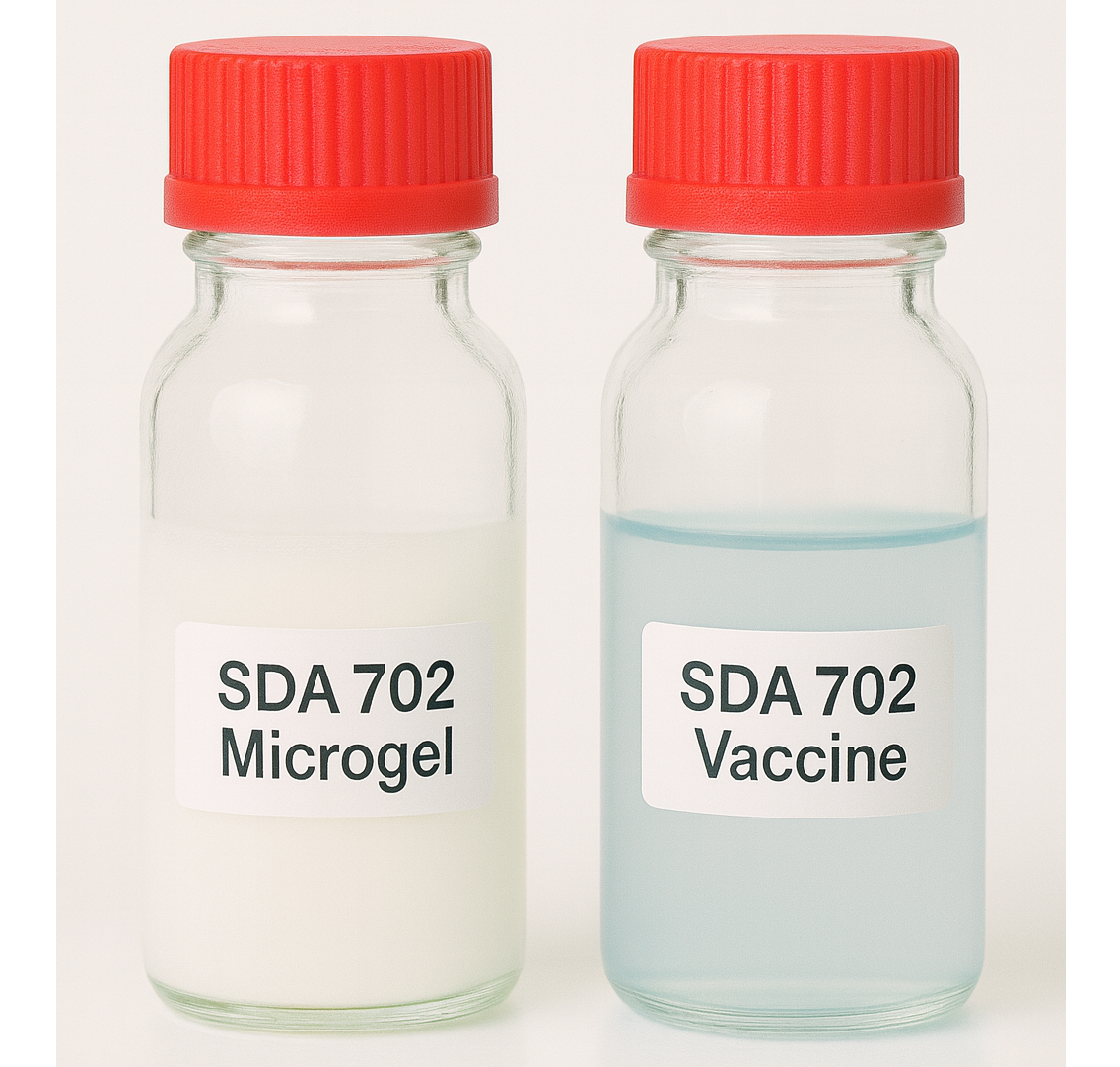
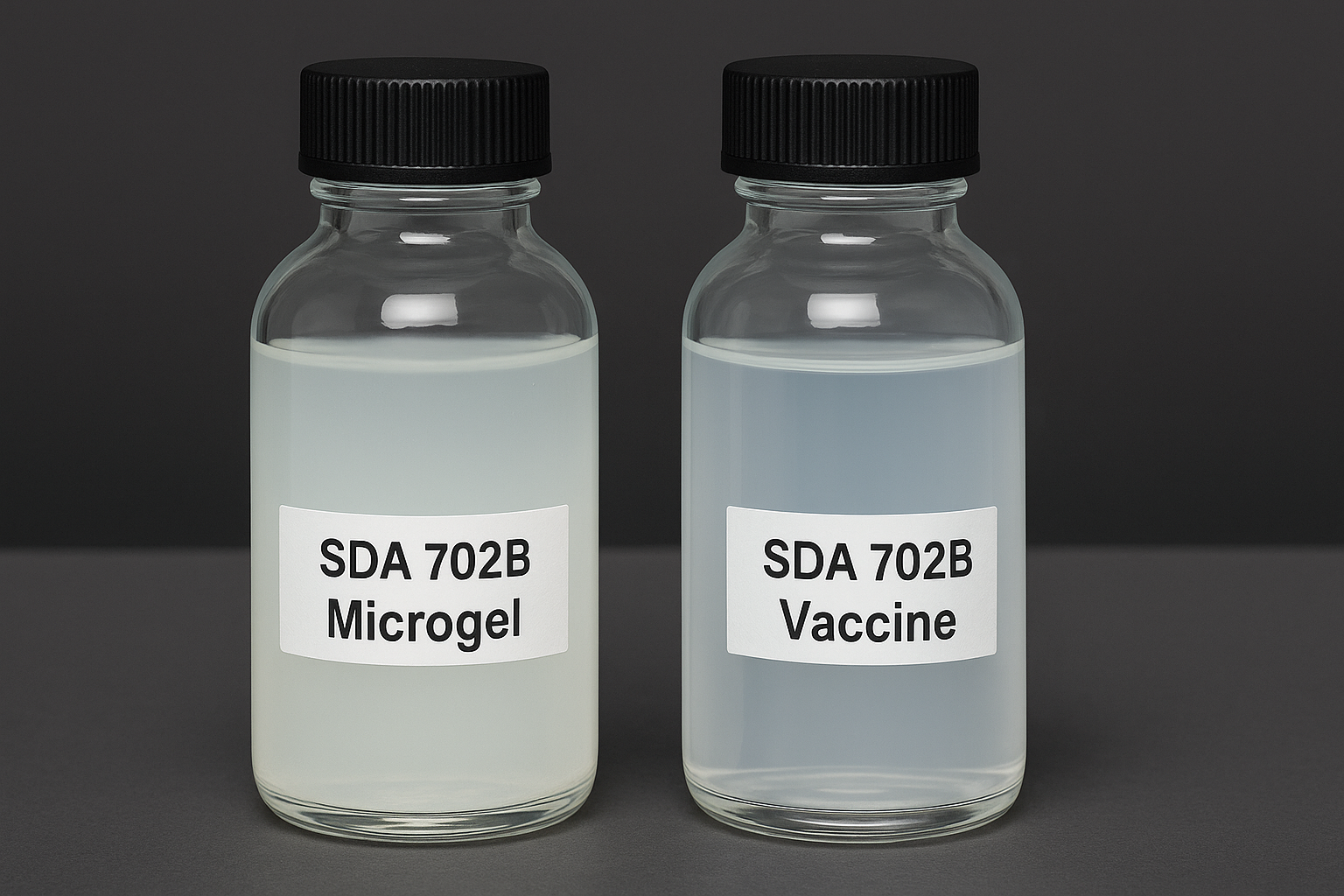
Advanced Vaccine Adjuvant Platform — Scientifically Engineered. Regulatory Ready. Commercial Proven

Microemulsion Immunosol System SDA7749, 4580, 6050
Small particle oil in water, provide extremely high antigen presentation and high safety. Colorless or…